A total of 63 deaths and 2,102 suspected cases of cholera have been recorded across 33 states and 122 local government areas in the country as of June 30, 2024, with a case fatality rate of 3.0% since the beginning of the year.
Ten states, including Lagos, Bayelsa, Abia, Zamfara, Bauchi, Katsina, Cross River, Ebonyi, Rivers, and Delta, account for about 90% of the cases, with seven of them in the southern part of the country.
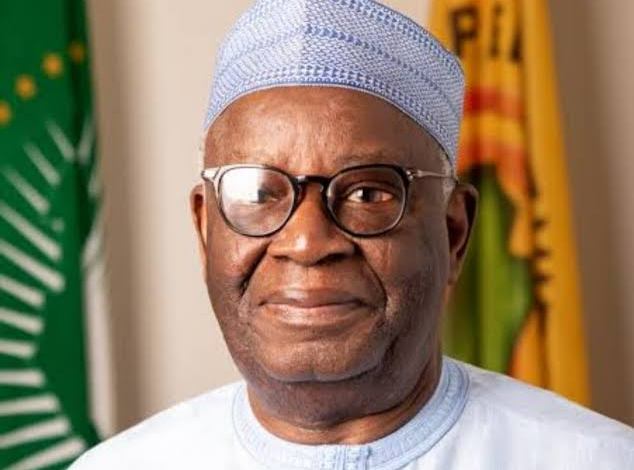
Director General of the Nigeria Centre for Disease Control and Prevention, Dr Jide Idris, who disclosed this yesterday in Abuja, observed that prior to the activation of the Emergency Operation Centre (EOC), the Nigeria Centre for Disease Control (NCDC), through the National Cholera Technical Working Group (NCTWG), had conducted assessments of cholera readiness and preparedness capacity in 22 hotspot and high-burden states. The report of identified gaps was shared with the states to guide their preparedness activities before the outbreak.
He identified some challenges being faced in the ongoing cholera response, including open defecation, inadequate toilet facilities, inadequate safe water, and poor sanitation. He added that only 123 (16%) of 774 LGAs in Nigeria are open defecation-free.
“With Jigawa as the only open defecation-free state in Nigeria, more than 48 million Nigerians practise open defecation. There are also issues with inadequate toilet facilities, even in many government facilities, which are not well maintained. Inadequate safe water and poor sanitation affect 11% of schools, 6% of health facilities, and 4% of motor parks and markets. Poor waste management practices, poor food, environmental, and personal hygiene practices contribute to the problem.”
READ ALSO:Bauchi records 50 suspected cholera cases in three LGAs
Idris noted a capacity gap among healthcare workers at the state and LGA levels, as well as weak regulation on the construction of soakaways and boreholes (some sunk close to water sources or in improper locations).
“We have inadequate capacity at the state level — delayed disease reporting and response actions, a capacity gap among healthcare workers at the state and LGA levels, poor regulation of food vendors and commercial water supply on hygiene, and weak regulation on the sighting of boreholes and wells close to sewage or toilet pathways.”
He said that the centre has provided relevant guidelines, SOPs, and advisories to states to enhance their technical readiness and response to the outbreak, as well as, prepositioning and distribution of medical supplies for case management, infection prevention, and control, and laboratory diagnosis have been conducted across all 36 states and the Federal Capital Territory (FCT).
Idris observed that the National Cholera Multisectoral Emergency Operation Centre (EOC) has been activated, which includes subject matter experts for strategic coordination. They meet daily to provide periodic situation reports for stakeholders, ensuring effective mobilisation, harmonisation, and distribution of resources to support affected states.
He said, “This is done through relevant thematic areas of response covering coordination, surveillance, case management, infection prevention and control, risk communication and community engagement, water sanitation and hygiene, vaccination, logistics, and research with a cost Incidence Action Plan being developed and implemented. These efforts will facilitate rapid communication, data analysis, decision-making, resource deployment efficiency, surveillance and diagnostic capacity strengthening, treatment enhancement for affected persons, and intensified public awareness and community engagement activities.”
The NCDC boss said the Centre has provided offsite/onsite technical support to states and follows up for daily reporting and progress with response activities. They continue sub-national level training of laboratory scientists on sample collection and analysis, and community mobilizers on cholera key messages. Capacity building has also been supported for LGA disease surveillance and notification officers across the country.
According to him, the NCDC has supported capacity building for LGA risk communication, community engagement, and health promotion officers nationwide. They have provided public health advisories and engaged regularly with the media to sensitise the general public on the need to take responsibility and play their part in breaking the transmission chain of this outbreak.
He said, “It is pertinent to acknowledge and highlight the strong political will to control the outbreak as demonstrated by Mr President’s constitution of an inter ministerial cabinet committee (including ministers of health, environment, water resources and sanitation, education, information and national orientation youth, aviation, women affairs, budget & planning, special duties and intergovernmental affairs, finance), to support the ongoing control effort, especially through specific relevant interventions relating to their ministries and agencies.”

 4 months ago
6
4 months ago
6











 English (US) ·
English (US) ·