The Federal Government has revealed that Healthcare-Associated Infections (HAIs) cost the country up to $4.5 billion in 2023. The National IPC Programme Coordinator, Dr Tochi Okwor, disclosed this during the inauguration of a national infection prevention and control (IPC) technical working group to improve patient safety and reduce healthcare-associated infections nationwide.
He stated that these infections occur due to suboptimal infection prevention and control in hospitals, and emphasised the importance of standardising procedures for preventing infectious diseases.
HAIs pose a significant threat to population health across the world and estimated that over 1.4 million people suffer from infectious complications acquired in hospitals. The infections acquired in the hospitals are due to resistant organisms.
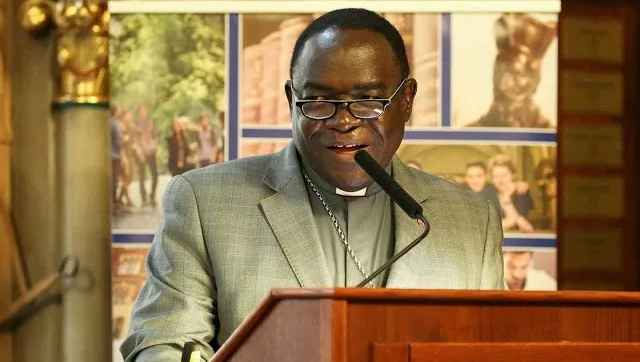
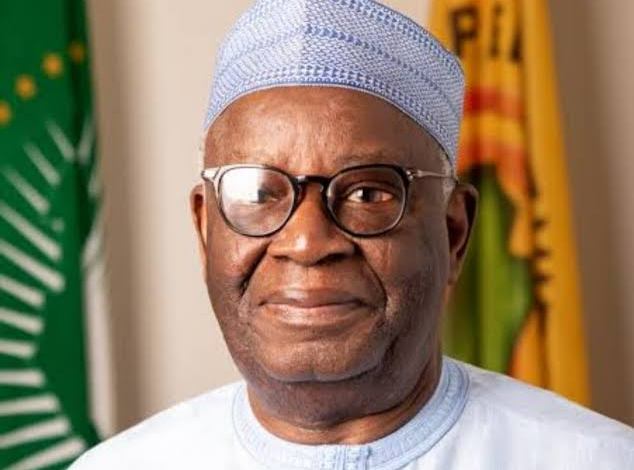
The Minister of Health and Social Welfare, Prof. Muhammad Pate, who inaugurated the technical working group in Abuja, said HAIs pose a significant threat to the health of Nigerians.
He noted that 44 per cent of patients admitted to the country’s hospitals acquire one of the HAIs during their stay. Pate lamented that the human and economic costs of these infections are substantial and cost $715 per episode, draining vital resources and funds that could be channelled towards other critical aspects of the health system.
According to him, the burden of associated infections goes beyond financial implications, as it represents a threat to the health and productive years of citizens, affecting the quality of life for countless families and healthcare workers.
The minister observed that these infections, caused by various pathogens, can lead to severe complications, extended hospital stays, and could tragically end in death.
He noted that the recent Joint External Evaluation (JEE) conducted in Nigeria indicated that while the country has made significant progress in infection prevention and control, there are still strategic areas that need to be strengthened.
NCDC Director General, Dr Jide Idris, said compelling evidence shows that up to 70 per cent of HAIs could be prevented by implementing effective IPC interventions.
He said IPC is not merely a set of protocols but is the cornerstone of public health and the bedrock upon which a resilient health system is built. Idris, represented by the Director, Public Health, Federal Ministry of Health, Dr Chukwuma Anyaike, said major outbreaks of diseases such as Ebola, Lassa fever, cerebrospinal meningitis, diphtheria, cholera, and the COVID-19 pandemic have demonstrated how rapidly infections can spread through communities and be amplified in healthcare settings.
He said: “These events have exposed gaps in our IPC programmes and highlighted the necessity for comprehensive infection prevention and antimicrobial resistance (AMR) strategies. No pa- tient seek ing care should be infected while receiving it and no healthcare worker should risk infection while providing care.”
Also speaking, the Dental Officer and Epidemiologist at the U.S. Centre for Disease Control and Prevention, Dr Farah Husain, said that robust IPC programmes are essential not only for protecting patients and healthcare workers but also for establishing sustainable systems that curb antimicrobial resistance and prevent outbreaks.

 3 months ago
38
3 months ago
38











 English (US) ·
English (US) ·